Site uses cookies.
Learn moreWhat to know about psoriasis
12 August 2022
Psoriasis is an inflammatory skin condition that can appear in many forms. Learn everything you need to know about the types of psoriasis here.
Psoriasis is an autoimmune condition that causes cells to develop rapidly on the skin. This overgrowth can lead to thick, scaly plaques that may itch or cause discomfort.
There are several different types of psoriasis. These vary depending on the appearance of the scales and their location on the body. In the United States, over 8 million people have a form of psoriasis.
Environmental triggers often cause the symptoms of psoriasis to flare. Although it is not currently possible to cure these symptoms, recent developments in psoriasis treatments mean that it is possible to reduce the number of flares and their severity.
This article will explain the different types of psoriasis, including their symptoms and how to treat them.
Symptoms
Psoriasis causes a buildup of skin cells on the skin’s surface, which leads to scaly patches of skin.
On light skin tones, psoriasis usually appears as pink or red patches with silvery white scales. On dark skin, psoriasis is more likely to appear as purple or dark brown patches with gray scales.
Psoriasis symptoms can alternate between periods of flares, during which they are intense, and remission, during which they clear up. Remission periods last for an average of 1–12 months at a time.
However, the duration of both flares and periods of remission can be challenging to predict.
A person’s symptoms can range from mild to severe, and they may present differently according to the type of psoriasis the person has.
According to the National Psoriasis Foundation:
Mild psoriasis covers less than 3% of the body.
Moderate psoriasis covers 3–10% of the body.
Severe psoriasis covers more than 10% of the body.
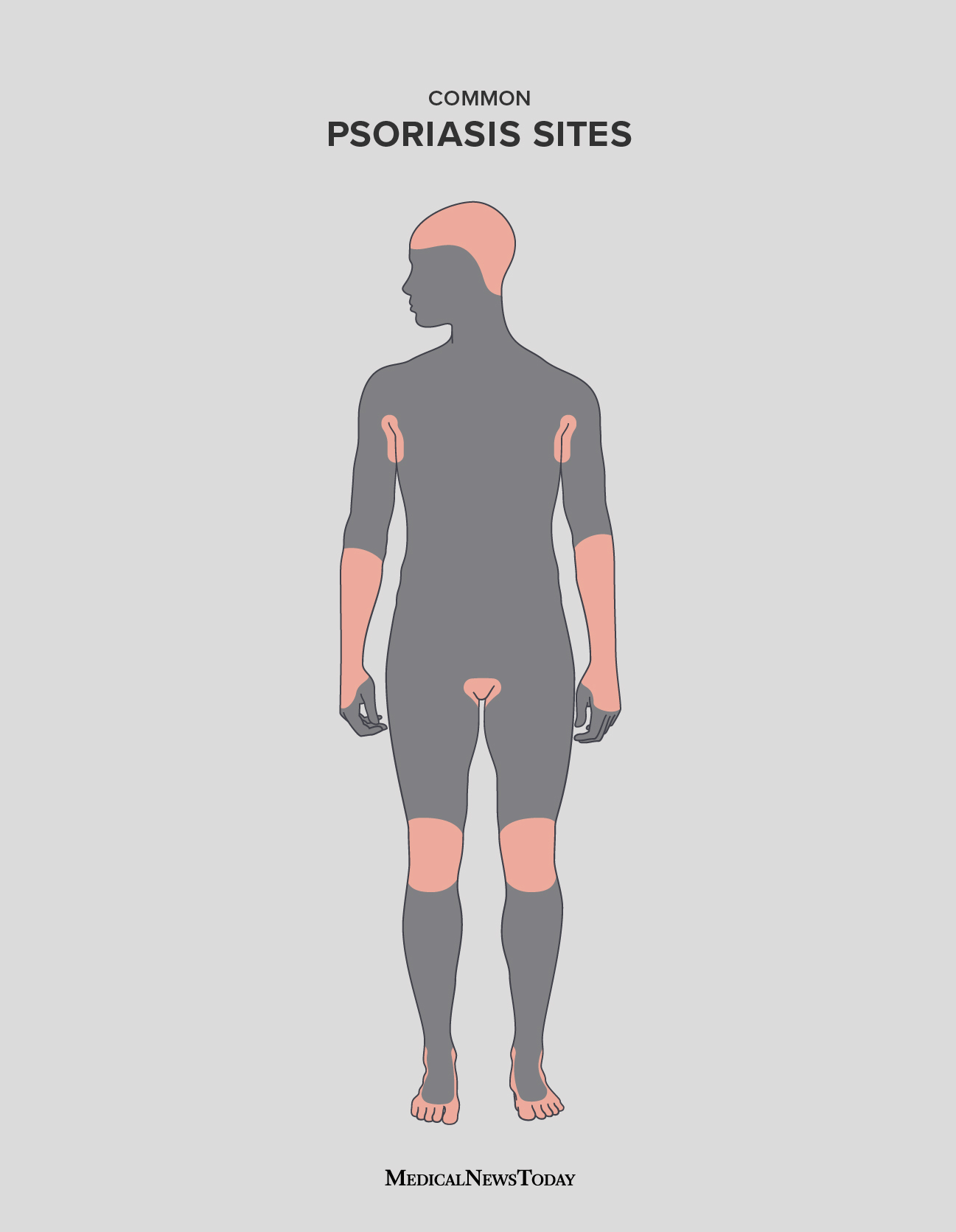
Plaques can develop anywhere, but they commonly occur as small patches on the elbows, knees, lower back, and scalp.
Types
There are several forms of psoriasis. The sections below will look at some of these in more detail.
Plaque psoriasis
About 80–90% of people with psoriasis have plaque psoriasis. On light skin, this usually shows as raised, inflamed, red lesions that are covered by silvery-white scales. On dark skin, it presents as purple or dark brown patches with gray scales.
Plaque psoriasis occurs most often on the elbows, knees, scalp, and lower back.
Inverse psoriasis
Inverse psoriasis is a variant of psoriasis that develops in skin folds. It commonly affects:
- the armpits
- the groin
- the areas under the breasts
- other skin folds, such as those around the genitals and buttocks
Inverse psoriasis typically produces lesions without the scales that occur in plaque psoriasis. The lesions might be smooth and shiny.
Irritation from rubbing and sweating can make this type of psoriasis worse due to its location in skin folds and tender areas. It is more common among people who are overweight and those with deep skin folds.
Erythrodermic psoriasis
Erythrodermic psoriasis is a type of psoriasis that can cause large areas of inflammation across the body. The condition is rare and affects around 1% to 2.25% of people with psoriasis.
In addition to severe inflammation, a person with erythrodermic psoriasis may experience severe itching, pain, and large-scale skin shedding.
Erythrodermic psoriasis also disrupts the body’s chemical balance. This interference may cause protein and fluid loss that can lead to the person developing severe complications such as pneumonia and congestive heart failure.
Edema, or swelling from fluid retention, may also occur, especially around the ankles. The body may also have difficulty regulating its temperature, which can cause shivering.
The complications of erythrodermic psoriasis can be dangerous. Anyone with any symptoms of this condition should contact a doctor right away. A person with erythrodermic psoriasis may need to spend time in the hospital if the symptoms are severe.
Guttate psoriasis
Guttate psoriasis is more common in children and adolescents than adults. It accounts for less than 30% of all cases of psoriasis.
It appears as small, individual spots on the skin. The spots are not usually as thick or as crusty as the lesions in plaque psoriasis.
A range of conditions can trigger guttate psoriasis, including:
- upper respiratory infections
- streptococcal infections
- tonsillitis
- stress
- injury to the skin
certain medications, including antimalarials, lithium, and beta-blockers
Guttate psoriasis may resolve without treatment and never return. However, it may clear up and reappear later as patches of plaque psoriasis.
Pustular psoriasis
Pustular psoriasis is a rare form of psoriasis that appears as white pustules, or blisters of pus, surrounded by inflamed skin. It can affect specific areas of the body, such as the hands and feet, or present more generally. It is not an infection, and it is not contagious.
Pustular psoriasis tends to have a cycle in which the formation of pustules and scaling follows the discoloration of the skin.
Although psoriasis can form anywhere on the human body, below are some of the most common areas.
Complications
Other health problems may develop as a result of psoriasis. Although some people think of it as a skin condition, psoriasis can also affect the bones, muscles, and metabolic system.
The sections below will look at some complications of psoriasis in more detail.
Psoriatic arthritis
Around 20–30% of people with psoriasis have joint inflammation with symptoms of arthritis. Collectively, this is known as psoriatic arthritis.
This type of psoriasis causes progressive damage to the joints. It is most common in people aged 30–50 years.
Other complications
People with psoriasis may experience social exclusion, self-image issues, and low self-esteem. Together with the physical discomfort, itching, and pain of psoriasis, these additional complications can affect their overall quality of life.
The social and physical demands of this chronic condition may also contribute to depression and anxiety.
Psoriasis might also lead to a higher risk of cardiovascular disease, metabolic syndrome, diabetes, and some types of cancer, including lung and non-melanoma skin cancer.
Causes and triggers
Although the cause of psoriasis is still unclear, scientists believe that it is an autoimmune condition. Autoimmune conditions affect the immune system, which produces T cells to protect the body against infectious agents.
In people with psoriasis, triggers can lead to their genes instructing the immune system to target the wrong cells. T cells respond to a trigger as if they are fighting an infection or healing a wound. They produce chemicals that cause inflammation.
In psoriasis, this autoimmune activity leads to the excessive growth of skin cells. Typically, skin cells take about 1 month to replace themselves. However, in people with psoriasis, they take around 3–4 days to do this.
Triggers will be different in each individual with psoriasis, but some common triggers include:
- stress and anxiety
- skin injuries
- infections
- hormonal changes
Medications that can trigger a psoriasis flare include:
- lithium
- antimalarials
- quinidine
- indomethacin
Importantly, psoriasis is not contagious. Knowing and remembering this can help people with the condition cope with the parts of socializing that they may find difficult.
Risk factors
Both external and internal factors can increase the risk of a person developing psoriasis.
Some risk factors for developing psoriasis include:
- cardiovascular disease
- metabolic syndrome
- trauma to the skin
- hypertension
- diabetes
- infection
- obesity
Genetics can play an important role in the formation of psoriasis. Studies have found more than 60 genetic markers linked to Th17 cell activation, which is a key component of inflammation in psoriasis.
As a result, a person’s family history may affect their risk of developing psoriasis. In fact, around 40% of people with psoriasis or psoriatic arthritis have a family history of either condition.
Among younger people, psoriasis may flare after an infection. Some common respiratory infections include strep throat, bronchitis, and tonsillitis.
Psoriasis is equally common among males and females. It can begin at any age, but it is most common in people aged 15–25 years. The average time of onset is 28 years of age. That said, around one-third of people with psoriasis develop it in childhood.
Is psoriasis contagious?
Psoriasis is an autoimmune condition that develops within the body. Certain triggers can cause psoriasis to appear in its first instance or worsen existing systems.
However, psoriasis is not contagious. A person cannot catch psoriasis.
Diagnosis
There are currently no blood tests that can confirm psoriasis, so a doctor will diagnose the condition by assessing a person’s rashes and lesions. The appearance of the symptoms may vary depending on the severity of the condition and the type of psoriasis the person has.
The doctor will examine the symptoms and ask about the individual’s personal and family history. They might also carry out a skin biopsy to rule out other conditions, such as eczema.
A person who has a persistent rash that does not resolve with over-the-counter (OTC) remedies may want to talk with a doctor. Often, recognizing and treating the symptoms early improves the long-term outcome associated with psoriasis.
Treatments
If a doctor confirms that a person has psoriasis, treatment will depend on the type and severity of the condition. The main options include medications and phototherapy.
People with psoriasis should use emollients to keep the skin moisturized when using other treatments. This precaution can help reduce the itching and irritation and may also reduce the number of lesions or plaques that develop.
Medications
Many topical, oral, and injected medications are available for people with psoriasis.
Some OTC remedies can help relieve the symptoms of very mild psoriasis. These include:
Coal tar: This can help soothe plaque psoriasis, itching, and lesions on the scalp, palms, and soles. People can use coal tar on its own or alongside another treatment.
Hydrocortisone creams: These reduce inflammation and soothe itching.
Salicylic acid: This can help reduce swelling and remove scales, often in people with scalp psoriasis.
Anti-itch agents: These include products containing calamine, hydrocortisone, camphor, or menthol.
Topical therapies
People apply topical treatments directly to the skin. This option is usually the first-line treatment for mild-to-moderate symptoms, and it aims to slow down the growth of skin cells, reduce inflammation, and soothe itching or discomfort.
These treatments are available over the counter or with a prescription, and they include nonsteroids and steroids. More specifically, examples include:
Corticosteroids: Doctors often recommend corticosteroids to help treat psoriasis symptoms. There are many different steroids available as gels, foams, creams, sprays, and ointments. The National Psoriasis Foundation offers a guide on understanding corticosteroid strengths here.
Synthetic vitamin D: People often use this alongside a corticosteroid. It can help flatten plaques, slow the growth of skin cells, and remove scales.
Retinoids: This is synthetic vitamin A that can help slow the growth of skin cells, reduce discoloration, and soothe itching. People commonly combine tazarotene, a topical retinoid, with corticosteroid treatment.
Pimecrolimus cream and tacrolimus ointment: These are steroid sparing eczema treatments that a doctor may prescribe to help reduce the symptoms of inverse and plaque psoriasis. People often combine them with a course of steroids.
Systemic therapies
Systemic therapies work through the whole body system. Doctors prescribe them for people who have moderate-to-severe psoriasis and psoriatic arthritis. They help reduce disease progression and the regularity of flares.
The following sections will look at some systemic therapies in more detail.
Biologics
These are protein-based drugs that derive from living cells. Biologics target the T cells and immune proteins that cause psoriasis and psoriatic arthritis.
The Food and Drug Administration (FDA) has approved multiple biologics. These include etanercept, infliximab, and adalimumab.
However, people should consider costs when seeking biologic treatment, and it is sensible to speak with an insurance provider about potential coverage.
Methotrexate
Doctors prescribe methotrexate for extremely severe psoriasis that restricts daily function and does not respond to any other treatments. Methotrexate is effective for psoriatic arthritis, as well as erythrodermic, palmoplantar, and nail psoriasis.
Cyclosporine
Doctors usually prescribe cyclosporine for preventing the rejection of organs after transplants. However, it can also help people with severe presentations of the following types of psoriasis:
- plaque
- guttate
- erythrodermic
- generalized pustular
- palmoplantar
- Oral retinoids
People with severe psoriasis can take a drug called acitretin, which works against the effects of the condition throughout the body. Acitretin does not reduce immune activity, making it safer for people with HIV who also have severe psoriasis.
People with all types of psoriasis except inverse psoriasis may benefit from using oral retinoids.
Off-label medications
Doctors may prescribe certain off-label medications if the standard FDA-approved drugs have not resolved a person’s symptoms or if the individual has another condition that prevents the use of specific medications.
However, due to several safe biologics recently coming to market, this is now a less common approach.
Phototherapy
Phototherapy involves regularly exposing the skin to certain lights and lasers under medical supervision. The light can slow cell growth, suppress immune activity, and reduce irritation.
People can carry out phototherapy at home using a lightbox or handheld device if their initial treatment is successful. Some people may also need to take psoralen pills before exposure to make their skin more sensitive to light.
Anyone who has coexisting conditions that make them sensitive to light, such as lupus or previous instances of skin cancer, should not use phototherapy.
Home remedies
It is not possible to avoid psoriasis flares. However, a person may be able to reduce their risk of flares by mitigating outside risk factors. These strategies can work alongside traditional treatment plans.
Some strategies include:
- reducing stress with yoga, exercise, and meditation
- eating a balanced diet
- recognizing and avoiding food triggers
- not smoking or drinking alcohol in excess
A person may also be able to use topical home remedies to reduce symptoms such as itching. They may do so by keeping the skin moisturized and avoiding hot, prolonged showers.
Although psoriasis can sometimes be isolating and uncomfortable, people have many options for managing the symptoms and treating the immune activity of the condition.
Psoriasis diet
There is no specific diet that can cure psoriasis. However, according to the National Psoriasis Foundation, eating a healthy diet may help a person with psoriasis manage their symptoms and reduce the risk of developing certain complications.
Inflammation is a main symptom of psoriasis. Certain food choices can help reduce or even prevent inflammation in the body. Maintaining a healthy diet may also reduce the risk of developing complications such as diabetes, high blood pressure, and heart disease.
The National Psoriasis Foundation recommends that people with the condition eat a varied, healthy diet that includes:
- limiting alcohol intake
- prioritizing lean protein sources, such as chicken breast
- eating fish rich in omega-3 fatty acids
- reducing gluten intake, if a person has a gluten allergy
- avoiding pro-inflammatory foods, such as simple carbohydrates and saturated fats
Summary
Psoriasis is an autoimmune condition that causes the body to produce skin cells at an increased rate. These cells then build up on the skin, forming plaques.
There are multiple types of psoriasis, ranging from small, itchy patches to severe rashes that can cover large parts of the body. More than 8 million people in the U.S. have a form of psoriasis.
The root cause of psoriasis is unclear. However, many environmental triggers — including stress and hormonal changes — can cause symptom flares.
Although there is no definitive cure for the condition, recent developments in psoriasis treatments mean that people can reduce the number of flares they experience and their severity.
Treatments for mild cases of psoriasis include topical ointments and lifestyle adjustments. However, in severe cases, rheumatologists may prescribe more advanced treatments, such as corticosteroids, retinoids, biologics, or phototherapy.
Article Source: https://www.medicalnewstoday.com/articles/52457#_noHeaderPrefixedContent



